Prevention and Management of Positional Cranial Deformities in Infancy
Beyond Cosmesis: Why It Matters
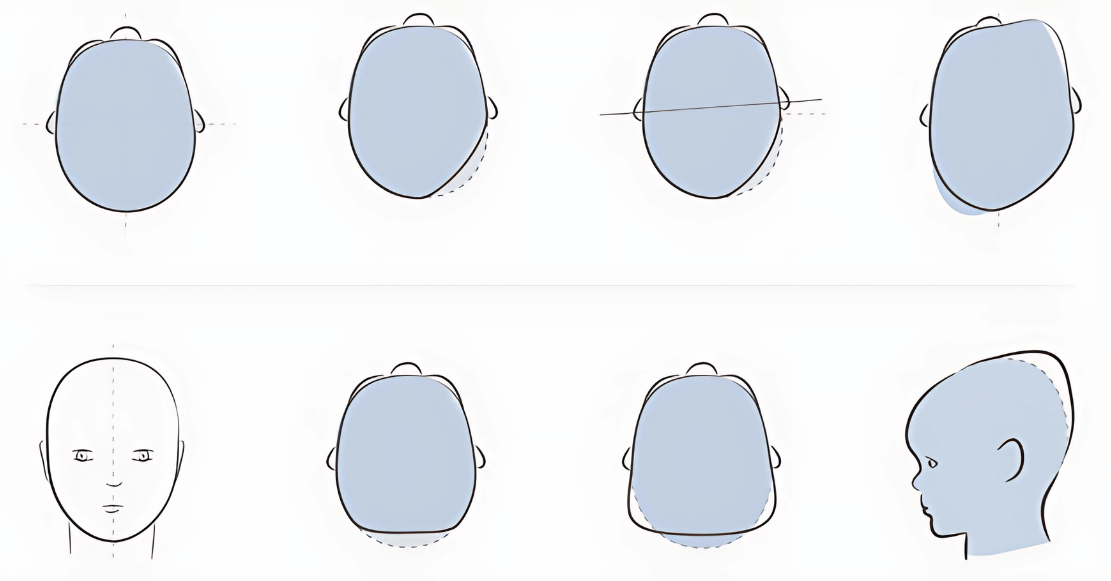
While PCDs are not life-threatening, their long-term aesthetic, psychological, and developmental impact should not be overlooked. Persistent asymmetries can affect jaw alignment, vision, and even auditory processing. Some studies also link PCDs with motor or neurodevelopmental delays, though causality remains debated.
Prevention: The Most Powerful Tool
Given the skull’s plasticity in early life, prevention should begin from day one. Evidence-based strategies include:
- Alternating head position during sleep.
- Encouraging tummy time from the first weeks.
- Alternating feeding sides.
- Carrying babies in slings or arms to reduce pressure.
- Using visual or auditory cues to promote head turning to both sides.
Pressure-relieving devices like the Medibino®, developed by craniofacial surgeon Dr. Susanne Kluba, support these strategies. It’s a certified, low-profile device suitable for prams and bassinets, shown to reduce severity and progression of PCDs.
Therapeutic Approaches
When deformities are established, early intervention is key:
- Physiotherapy and manual therapy are first line for torticollis or motor delays.
- Positioning therapy may help moderate cases.
- Helmet therapy may be recommended in severe cases, ideally started between 5–6 months before cranial growth slows.
Referral to a craniofacial specialist is advised if:
- Deformities persist beyond 4 months.
- There is no improvement with conservative measures.
- There are concerns about synostosis.
Conclusion
Recognising the signs of PCDs and offering early guidance is essential for healthcare professionals. Whether through repositioning, therapy, or cranial orthoses, early identification and proactive care can reduce the need for invasive treatments and support optimal neurodevelopmental outcomes.